Making Water Safe in an Emergency
Boil Water Advisory Fact Sheet
E. coli Contamination/Water Supply Interruption at Food Establishments
Making Water Safe in an Emergency Boil Water Advisory Fact Sheet E. coli Contamination/Water Supply Interruption at Food Establishments Bulk Water Hauling at Food Establishments
The following content is from the CT DPH on April 12, 2024 and was not written by HVHD. HARTFORD, Conn— On April 10, the United States Environmental Protection Agency (EPA) announced the Final National Primary Drinking Water Rule (NPDWR) for Per- and Polyfluoroalkyl Substances (PFAS). This first-ever national, legally enforceable drinking water standard will protect communities from exposure to
EPA announces drinking water standards regarding harmful PFAS substances Read More »
The following content is from the CT DPH on April 12, 2024 and was not written by HVHD.
HARTFORD, Conn— On April 10, the United States Environmental Protection Agency (EPA) announced the Final National Primary Drinking Water Rule (NPDWR) for Per- and Polyfluoroalkyl Substances (PFAS). This first-ever national, legally enforceable drinking water standard will protect communities from exposure to harmful PFAS which also are known as “forever chemicals.” The science is clear: exposure to certain PFAS can have negative health impacts, and EPA is using the latest science to establish national drinking water standards.
The new EPA NPDWR for PFAS sets regulatory limits called maximum contaminant levels (MCL) for six PFAS in public drinking water. It also requires that public water systems monitor for PFAS, provide customer notification, and report to the Connecticut Department of Public Health (DPH) if PFAS are detected. Water companies are also required to reduce customers’ exposure to PFAS in drinking water if levels exceed the MCL.
MCLs for PFAS per EPA’s new rule are as follows:
:
| Analyte | EPA MCL(parts per trillion, ppt, ng/L) |
| Perfluorooctanoic acid (PFOA) | 4 |
| Perfluorooctane sulfonic acid (PFOS) | 4 |
| Perfluorononanoic acid (PFNA) | 10 |
| Perfluorohexane sulfonic acid (PFHxS) | 10 |
| Hexafluoropropylene oxide dimer acid(HFPO-DA / GenX) | 10 |
| Mixture of two or more of the following:PFNAPFHxSHFPO-DA / GenXPerfluorobutane sulfonic acid (PFBS) | Hazard Index* of 1 |
| *Hazard Index (HI): The Hazard Index is a long-established approach that EPA regularly uses to understand health risk from a chemical mixture (i.e., exposure to multiple chemicals). The HI is made up of a sum of fractions. Each fraction compares the level of each PFAS measured in the water to their respective health-based water concentration. For additional information on the HI please see the following link from EPA: https://www.epa.gov/system/files/documents/2024-04/pfas-npdwr_fact-sheet_hazard-index_4.8.24.pdf | |
Public water systems are required to comply with the new NPDWR within five years of implementation. In the coming weeks, DPH will provide an estimated timeline for adopting this rule in Connecticut and recommendations to public water systems to prepare for implementation. DPH also will update its web pages for PFAS Frequently Asked Questions and PFAS Information for Public Water Systems which includes acknowledging the difference between the new MCLs and the Connecticut Drinking Water Action Levels for these compounds.
“Connecticut recognizes the public health threat posed by PFAS, and as a result of Governor Ned Lamont’s Interagency PFAS Task Force PFAS Action Plan, we can protect all residents, including sensitive populations, from adverse health effects due to a lifetime of exposure to these chemicals in drinking water,” said Connecticut Department of Public Health Commissioner Manisha Juthani, MD, who co-chairs the State’s PFAS Task Force. “The EPA’s decision to set enforceable limits for PFAS in public drinking water is a welcome tool that our agency can use to ensure that consumers of public drinking water are protected from these PFAS chemicals. Connecticut’s individual PFAS action levels also are consistent with the range of drinking water guidelines and standards recently established by other states, including neighboring states in the northeast.”
Commissioner Juthani added that thanks to the Bipartisan Infrastructure Law, there is a historic amount of federal funding for addressing PFAS in drinking water. To learn more about how DPH has proposed to utilize this funding to assist public water systems, including those serving small or disadvantaged communities, please visit DPH’s Drinking Water State Revolving Fund Final Intended Use Plans for 2023 and 2024.
PFAS are a group of thousands of manufactured chemicals with many beneficial properties including the ability to repel water, prevent staining, and increase heat resistance. PFAS have many industrial and consumer uses including fabric, carpet, electrical wire and non-stick coatings, food packaging, and firefighting foam used to extinguish petroleum fires.
However, toxicological studies in laboratory animals consistently show effects on the liver and immune system, and on growth, reproduction, and fetal development. PFAS can also impact the endocrine (e.g. thyroid) and hormonal systems and can disturb blood lipids such as cholesterol.
PFAS are not readily absorbed through the skin so bathing, showering, swimming, and washing dishes in water containing PFAS are not significant sources of exposure. But consuming PFAS-contaminated drinking water over many years can cause such chemicals to accumulate in the body and make it more likely for adverse health effects to occur.
Additional information and resources can be found at the EPA Factsheet for the PFAS National Primary Drinking Water Regulation. For information on DPH’s drinking water action levels and answers to some frequently asked questions, please refer to DPH’s PFAS Information Webpage.
As part of the Administration’s commitment to combating PFAS pollution, EPA announces $1B investment through President Biden’s Investing in America agenda to address PFAS in drinking water The following content is from the EPA on April 1, 2024 and was not written by HVHD. HVHD is awaiting additional guidance and information from CT DPH. Reach
The following content is from the EPA on April 1, 2024 and was not written by HVHD.
HVHD is awaiting additional guidance and information from CT DPH. Reach out to Amy Bethge (abethge@hvhdct.gov) or DEEP if you have concerns regarding your water.
WASHINGTON – Today, April 10, the Biden-Harris Administration issued the first-ever national, legally enforceable drinking water standard to protect communities from exposure to harmful per-and polyfluoroalkyl substances (PFAS), also known as ‘forever chemicals.’ Exposure to PFAS has been linked to deadly cancers, impacts to the liver and heart, and immune and developmental damage to infants and children. This final rule represents the most significant step to protect public health under EPA’s PFAS Strategic Roadmap. The final rule will reduce PFAS exposure for approximately 100 million people, prevent thousands of deaths, and reduce tens of thousands of serious illnesses. Today’s announcement complements President Biden’s government-wide action plan to combat PFAS pollution.
Through President Biden’s Investing in America agenda, EPA is also making unprecedented funding available to help ensure that all people have clean and safe water. In addition to today’s final rule, EPA is announcing nearly $1 billion in newly available funding through the Bipartisan Infrastructure Law to help states and territories implement PFAS testing and treatment at public water systems and to help owners of private wells address PFAS contamination. This is part of a $9 billion investment through the Bipartisan Infrastructure Law to help communities with drinking water impacted by PFAS and other emerging contaminants – the largest-ever investment in tackling PFAS pollution. An additional $12 billion is available through the Bipartisan Infrastructure Law for general drinking water improvements, including addressing emerging contaminants like PFAS.
EPA Administrator Michael Regan will join White House Council on Environmental Quality Chair Brenda Mallory to announce the final standard today at an event in Fayetteville, North Carolina. In 2017, area residents learned that the Cape Fear River, the drinking water source for 1 million people in the region, had been heavily contaminated with PFAS pollution from a nearby manufacturing facility. Today’s announcements will help protect communities like Fayetteville from further devastating impacts of PFAS.
“Drinking water contaminated with PFAS has plagued communities across this country for too long,” said EPA Administrator Michael S. Regan. “That is why President Biden has made tackling PFAS a top priority, investing historic resources to address these harmful chemicals and protect communities nationwide. Our PFAS Strategic Roadmap marshals the full breadth of EPA’s authority and resources to protect people from these harmful forever chemicals. Today, I am proud to finalize this critical piece of our Roadmap, and in doing so, save thousands of lives and help ensure our children grow up healthier.”
“President Biden believes that everyone deserves access to clean, safe drinking water, and he is delivering on that promise,” said Brenda Mallory, Chair of the White House Council on Environmental Quality. “The first national drinking water standards for PFAS marks a significant step towards delivering on the Biden-Harris Administration’s commitment to advancing environmental justice, protecting communities, and securing clean water for people across the country.”
“Under President Biden’s leadership, we are taking a whole-of-government approach to tackle PFAS pollution and ensure that all Americans have access to clean, safe drinking water. Today’s announcement by EPA complements these efforts and will help keep our communities safe from these toxic ‘forever chemicals,’” said Deputy Assistant to the President for the Cancer Moonshot, Dr. Danielle Carnival. “Coupled with the additional $1 billion investment from President Biden’s Investing in America agenda to help communities address PFAS pollution, the reductions in exposure to toxic substances delivered by EPA’s standards will further the Biden Cancer Moonshot goal of reducing the cancer death rate by at least half by 2047 and preventing more than four million cancer deaths — and stopping cancer before it starts by protecting communities from known risks associated with exposure to PFAS and other contaminants, including kidney and testicular cancers, and more.”
EPA is taking a signature step to protect public health by establishing legally enforceable levels for several PFAS known to occur individually and as mixtures in drinking water. This rule sets limits for five individual PFAS: PFOA, PFOS, PFNA, PFHxS, and HFPO-DA (also known as “GenX Chemicals”). The rule also sets a limit for mixtures of any two or more of four PFAS: PFNA, PFHxS, PFBS, and “GenX chemicals.” By reducing exposure to PFAS, this final rule will prevent thousands of premature deaths, tens of thousands of serious illnesses, including certain cancers and liver and heart impacts in adults, and immune and developmental impacts to infants and children.
This final rule advances President Biden’s commitment to ending cancer as we know it as part of the Biden Cancer Moonshot, to ensuring that all Americans have access to clean, safe, drinking water, and to furthering the Biden-Harris Administration’s commitment to environmental justice by protecting communities that are most exposed to toxic chemicals.
EPA estimates that between about 6% and 10% of the 66,000 public drinking water systems subject to this rule may have to take action to reduce PFAS to meet these new standards. All public water systems have three years to complete their initial monitoring for these chemicals. They must inform the public of the level of PFAS measured in their drinking water. Where PFAS is found at levels that exceed these standards, systems must implement solutions to reduce PFAS in their drinking water within five years.
The new limits in this rule are achievable using a range of available technologies and approaches including granular activated carbon, reverse osmosis, and ion exchange systems. For example, the Cape Fear Public Utility Authority, serving Wilmington, NC – one of the communities most heavily impacted by PFAS contamination – has effectively deployed a granular activated carbon system to remove PFAS regulated by this rule. Drinking water systems will have flexibility to determine the best solution for their community.
EPA will be working closely with state co-regulators in supporting water systems and local officials to implement this rule. In the coming weeks, EPA will host a series of webinars to provide information to the public, communities, and water utilities about the final PFAS drinking water regulation. To learn more about the webinars, please visit EPA’s PFAS drinking water regulation webpage. EPA has also published a toolkit of communications resources to help drinking water systems and community leaders educate the public about PFAS, where they come from, their health risks, how to reduce exposure, and about this rule.
“We are thankful that Administrator Regan and the Biden Administration are taking this action to protect drinking water in North Carolina and across the country,” said North Carolina Governor Roy Cooper. “We asked for this because we know science-based standards for PFAS and other compounds are desperately needed.”
“For decades, the American people have been exposed to the family of incredibly toxic ‘forever chemicals’ known as PFAS with no protection from their government. Those chemicals now contaminate virtually all Americans from birth. That’s because for generations, PFAS chemicals slid off of every federal environmental law like a fried egg off a Teflon pan — until Joe Biden came along,” said Environmental Working Group President and Co-Founder Ken Cook. “We commend EPA Administrator Michael Regan for his tireless leadership to make this decision a reality, and CEQ Chair Brenda Mallory for making sure PFAS is tackled with the ‘whole of government’ approach President Biden promised. There is much work yet to be done to end PFAS pollution. The fact that the EPA has adopted the very strong policy announced today should give everyone confidence that the Biden administration will stay the course and keep the president’s promises, until the American people are protected, at long last, from the scourge of PFAS pollution.”
“We learned about GenX and other PFAS in our tap water six years ago. I raised my children on this water and watched loved ones suffer from rare or recurrent cancers. No one should ever worry if their tap water will make them sick or give them cancer. I’m grateful the Biden EPA heard our pleas and kept its promise to the American people. We will keep fighting until all exposures to PFAS end and the chemical companies responsible for business-related human rights abuses are held fully accountable,” said Emily Donovan, co-founder of Clean Cape Fear.
More details about funding to address PFAS in Drinking Water
Through the Bipartisan Infrastructure Law, EPA is making an unprecedented $21 billion available to strengthen our nation’s drinking water systems, including by addressing PFAS contamination. Of that, $9 billion is specifically for tackling PFAS and emerging contaminants. The financing programs delivering this funding are part of President Biden’s Justice40 Initiative, which set the goal that 40% of the overall benefits of certain federal investments flow to disadvantaged communities that have been historically marginalized by underinvestment and overburdened by pollution.
Additionally, EPA has a nationwide Water Technical Assistance program to help small, rural, and disadvantaged communities access federal resources by working directly with water systems to identify challenges like PFAS; develop plans; build technical, managerial, and financial capacity; and apply for water infrastructure funding. Learn more about EPA’s Water Technical Assistance programs.
More details about the final PFAS drinking water standards:
EPA is issuing this rule after reviewing extensive research and science on how PFAS affects public health, while engaging with the water sector and with state regulators to ensure effective implementation. EPA also considered 120,000 comments on the proposed rule from a wide variety of stakeholders.
Background:
PFAS, also known as ‘forever chemicals,’ are prevalent in the environment. PFAS are a category of chemicals used since the 1940s to repel oil and water and resist heat, which makes them useful in everyday products such as nonstick cookware, stain resistant clothing, and firefighting foam. The science is clear that exposure to certain PFAS over a long period of time can cause cancer and other illnesses. In addition, PFAS exposure during critical life stages such as pregnancy or early childhood can also result in adverse health impacts.
Across the country, PFAS contamination is impacting millions of people’s health and wellbeing. People can be exposed to PFAS through drinking water or food contaminated with PFAS, by coming into contact with products that contain PFAS, or through workplace exposures in certain industries.
Since EPA Administrator Michael S. Regan announced the PFAS Strategic Roadmap in October 2021, EPA has taken action – within the Biden-Harris Administration’s whole-of-government approach – by advancing science and following the law to safeguard public health, protect the environment, and hold polluters accountable. The actions described in the PFAS Strategic Roadmap each represent important and meaningful steps to protect communities from PFAS contamination. Cumulatively, these actions will build upon one another and lead to more enduring and protective solutions. In December 2023, the EPA released its second annual report on PFAS progress. The report highlights significant accomplishments achieved under the EPA’s PFAS Strategic Roadmap.
The following content is from the CDC on April 1, 2024 and was not written by HVHD. April 1, 2024—A person in the United States has tested positive for highly pathogenic avian influenza (HPAI) A(H5N1) virus (“H5N1 bird flu”), as reported by Texas and confirmed by CDC. This person had exposure to dairy cattle in Texas presumed
The following content is from the CDC on April 1, 2024 and was not written by HVHD.
April 1, 2024—A person in the United States has tested positive for highly pathogenic avian influenza (HPAI) A(H5N1) virus (“H5N1 bird flu”), as reported by Texas and confirmed by CDC. This person had exposure to dairy cattle in Texas presumed to be infected with HPAI A(H5N1) viruses. The patient reported eye redness (consistent with conjunctivitis), as their only symptom, and is recovering. The patient was told to isolate and is being treated with an antiviral drug for flu. This infection does not change the H5N1 bird flu human health risk assessment for the U.S. general public, which CDC considers to be low. However, people with close or prolonged, unprotected exposures to infected birds or other animals (including livestock), or to environments contaminated by infected birds or other animals, are at greater risk of infection. CDC has interim recommendations for prevention, monitoring, and public health investigations of HPAI A(H5N1) viruses.
CDC is working with state health departments to continue to monitor workers who may have been in contact with infected or potentially infected birds/animals and test those people who develop symptoms. CDC also has recommendations for clinicians on monitoring, testing, and antiviral treatment for patients with suspected or confirmed avian influenza A virus infections.
This is the second person reported to have tested positive for influenza A(H5N1) viruses in the United States. A previous human case occurred in 2022 in Colorado. Human infections with avian influenza A viruses, including A(H5N1) viruses, are uncommon but have occurred sporadically worldwide. CDC has been monitoring for illness among people exposed to H5 virus-infected birds since outbreaks were first detected in U.S. wild birds and poultry in late 2021. Human illnesses with H5N1 bird flu have ranged from mild (e.g., eye infection, upper respiratory symptoms) to severe illness (e.g., pneumonia) that have resulted in death in other countries.
H5 bird flu is widespread among wild birds in the U.S. and globally. These viruses also have caused outbreaks in commercial and backyard poultry flocks, and sporadic infections in mammals. HPAI in dairy cows was first reported in Texas and Kansas by the U.S. Department of Agriculture (USDA) on March 25, 2024. Unpasteurized milk from sick cattle collected from two dairy farms in Kansas and one in Texas, as well as a throat swab from a cow in another dairy in Texas, tested positive for HPAI A(H5) viruses of the genetic clade 2.3.4.4b, which is the same clade that is widespread among birds globally. On March 29, 2024, USDA’s National Veterinary Services Laboratories (NVSL) confirmed HPAI in a Michigan dairy herd that had recently received cows from Texas. The USDA Animal and Plant Health Inspection Service (APHIS) is providing regular updates on detections in dairy herds, as well as information on epidemiological findings and biosecurity guidance for farmers and veterinarians. Preliminary analysis of A(H5N1) viruses has not found changes that would make these viruses resistant to current FDA-approved flu antiviral medications, so these are believed to be effective against these viruses. Candidate vaccine viruses (CVVs) developed against related clade 2.3.4.4b viruses are available for vaccine manufacturing if necessary and preliminary analysis indicates that they may provide reasonable protection against H5N1 influenza viruses. Seasonal flu vaccines do not provide protection against these viruses. Analysis of virus samples is ongoing.
CDC is working closely with state and federal agencies, including USDA, the Food and Drug Administration (FDA), and local health authorities to further investigate and closely monitor this situation.
Prevention Measures
According to CDC’s interim recommendations, people should avoid unprotected exposures to sick or dead animals including wild birds, poultry, other domesticated birds, and other wild or domesticated animals (including cattle), as well as with animal carcasses, raw milk, feces (poop), litter, or materials contaminated by birds or other animals with confirmed or suspected HPAI A(H5N1)-virus infection. People should not prepare or eat uncooked or undercooked food or related uncooked food products, such as unpasteurized (raw) milk, or products made from raw milk such as cheeses, from animals with confirmed or suspected HPAI A(H5N1)-virus infection (avian influenza or bird flu). Specific recommendations for farmers; poultry, backyard flock, and livestock owners; and worker protection are also available.
People exposed to birds or other animals with confirmed or suspected HPAI A(H5N1) virus infection should be monitored for any signs and symptoms of illness for 10 days after the last known exposure, including people wearing recommended personal protective equipment (PPE). Additional information on protective actions around birds, including what to do if you find a dead bird, is available on CDC’s website.
According to FDA and USDA, there are not concerns with the safety of the commercial milk supply at this time because products are pasteurized before entering the market. Dairies are required to send only milk from healthy animals into processing for human consumption; milk from impacted animals is being diverted or destroyed so that it does not enter the human food supply. In addition, pasteurization has continually proven to inactivate bacteria and viruses, like influenza, in milk. Pasteurization is required for any milk entering interstate commerce for human consumption. FDA’s longstanding position is that unpasteurized, raw milk can harbor dangerous microorganisms that can pose serious health risks to consumers, and FDA is reminding consumers of the risks associated with raw milk consumption in light of the HPAI detections.
CDC continues to work with USDA, FDA, and state health departments to monitor people exposed to animals infected with HPAI A(H5N1) viruses. Because influenza viruses constantly change, continued surveillance and preparedness efforts are critical, and CDC is taking measures in case the public health risk assessment changes. This is a developing situation, and CDC will share additional updates as new relevant information becomes available.
The following content is from the CT DPH on April 1, 2024 and was not written by HVHD. HARTFORD, Conn—Despite the first human case of highly pathogenic avian influenza (HPAI) A(H5N1) virus which was reported in Texas over the weekend in a person exposed to an infected dairy cow, officials from the Connecticut Department of
The following content is from the CT DPH on April 1, 2024 and was not written by HVHD.
HARTFORD, Conn—Despite the first human case of highly pathogenic avian influenza (HPAI) A(H5N1) virus which was reported in Texas over the weekend in a person exposed to an infected dairy cow, officials from the Connecticut Department of Public Health (DPH) and the Connecticut Department of Agriculture (DoAg) say there are no cases reported in any cattle or other livestock in Connecticut.
The patient in Texas—who experienced eye inflammation as their only symptom and is clinically improving—was tested for flu late last week with confirmatory testing performed by the CDC over the weekend. The patient is being treated with the antiviral drug Oseltamivir, and the case does not change the risk to the general public, which remains low. Additionally, officials stress the state’s commercial milk supply is safe, due to the pasteurization process which is required for interstate commerce.
According to CDC’s interim recommendations, people should avoid unprotected exposures to sick or dead animals including wild birds, poultry, other domesticated birds, and other wild or domesticated animals (including cattle), as well as with animal carcasses, raw milk, feces, litter, or materials contaminated by birds or other animals with confirmed or suspected HPAI A(H5N1)-virus infection.
People should not prepare or eat uncooked or undercooked food or related uncooked food products, such as unpasteurized (raw) milk, or products made from raw milk, such as cheeses from animals with confirmed or suspected HPAI A(H5N1)-virus infection (avian influenza or bird flu).
“This is an evolving situation in Texas. The current risk of infection from avian influenza to residents of Connecticut remains low. Because pasteurization kills pathogens, including avian influenza, in milk, residents of Connecticut should be reassured by the safety of drinking or eating pasteurized dairy products. While we have no evidence of human-to-human transmission at this time, we need to remain vigilant,” said DPH Commissioner Manisha Juthani, MD.
Commissioner Juthani added that while seasonal flu vaccines do not provide protection against HPAI A(H5N1)-virus infection, the CDC is working with state health departments to continue to monitor workers who may have been in contact with infected or potentially infected birds/animals and test those people who develop symptoms. CDC also has guidance for clinicians on monitoring, testing, and antiviral treatment for patients with suspected or confirmed avian influenza A virus infections. According to the CDC, this is the second human case of H5N1 flu in the United States and the first linked to an exposure to cattle.
On March 25, the U.S. Department of Agriculture (USDA), Food & Drug Administration (FDA) and the CDC confirmed positive test results for highly pathogenic avian influenza in Texas and Kansas dairy herds.
Based on the information and research available, there is no concern about the safety of the commercial milk supply or that this circumstance poses a risk to consumer health. Dairies are required to send only milk from healthy animals into processing for human consumption, and milk from affected animals is not entering the food supply. Pasteurization has continually proven to inactivate bacteria and viruses, like influenza, in milk.
“At this time, there are no confirmed cases of H5N1 in dairy cattle or other livestock in Connecticut. We are monitoring this situation as it evolves nationally and continue to amplify the information shared from federal partners on a local level,” said Connecticut DoAg Commissioner Bryan P. Hurlburt. “We encourage Connecticut producers to enhance their on-farm biosecurity measures for the health and safety of livestock and farm workers.”
In addition to enhancing biosecurity, Commissioner Hurlburt added that producers and veterinarians should report cases of sick cattle to State Animal Health Officials at 860-713-2505 or ctstate.vet@ct.gov.
The following content is from the CDC on March 18, 2024 and was not written by HVHD. SummaryThe Centers for Disease Control and Prevention (CDC) is issuing this Health Alert Network (HAN) Health Advisory to inform clinicians and public health officials of an increase in global and U.S. measles cases and to provide guidance on
The following content is from the CDC on March 18, 2024 and was not written by HVHD.
Summary
The Centers for Disease Control and Prevention (CDC) is issuing this Health Alert Network (HAN) Health Advisory to inform clinicians and public health officials of an increase in global and U.S. measles cases and to provide guidance on measles prevention for all international travelers aged ≥6 months and all children aged ≥12 months who do not plan to travel internationally. Measles (rubeola) is highly contagious; one person infected with measles can infect 9 out of 10 unvaccinated individuals with whom they come in close contact. From January 1 to March 14, 2024, CDC has been notified of 58 confirmed U.S. cases of measles across 17 jurisdictions, including seven outbreaks in seven jurisdictions compared to 58 total cases and four outbreaks reported the entire year in 2023. Among the 58 cases reported in 2024, 54 (93%) were linked to international travel. Most cases reported in 2024 have been among children aged 12 months and older who had not received measles-mumps-rubella (MMR) vaccine. Many countries, including travel destinations such as Austria, the Philippines, Romania, and the United Kingdom, are experiencing measles outbreaks. To prevent measles infection and reduce the risk of community transmission from importation, all U.S. residents traveling internationally, regardless of destination, should be current on their MMR vaccinations. Healthcare providers should ensure children are current on routine immunizations, including MMR. Given currently high population immunity against measles in most U.S. communities, the risk of widescale spread is low. However, pockets of low coverage leave some communities at higher risk for outbreaks.
Background
Measles is a highly contagious viral illness and can cause severe health complications, including pneumonia, encephalitis (inflammation of the brain), and death, especially in unvaccinated persons. Measles typically begins with a prodrome of fever, cough, coryza (runny nose), and conjunctivitis (pink eye), lasting 2 to 4 days before rash onset. The incubation period for measles from exposure to fever is usually about 10 days (range 7 to 12 days), while rash onset is typically visible around 14 days (range 7 to 21 days) after initial exposure. The virus is transmitted through direct contact with infectious droplets or by airborne spread when an infected person breathes, coughs, or sneezes, and can remain infectious in the air and on surfaces for up to 2 hours after an infected person leaves an area. Individuals infected with measles are contagious from 4 days before the rash starts through 4 days afterward.
Declines in measles vaccination rates globally have increased the risk of measles outbreaks worldwide, including in the United States. Measles cases continue to be brought into the United States by travelers who are infected while in other countries. As a result, domestic measles outbreaks have been reported in most years, even following the declaration of U.S. measles elimination in 2000. Most importations come from unvaccinated U.S. residents.
Measles is almost entirely preventable through vaccination. MMR vaccines are safe and highly effective, with two doses being 97% effective against measles (one dose is 93% effective). When more than 95% of people in a community are vaccinated (coverage >95%) most people are protected through community immunity (herd immunity). However, vaccination coverage among U.S. kindergartners has decreased from 95.2% during the 2019–2020 school year to 93.1% in the 2022–2023 school year, leaving approximately 250,000 kindergartners susceptible to measles each year over the last three years. Thirty-six states plus the District of Columbia (DC) had less than 95% MMR coverage among kindergartners during the 2022–2023 school year. Of states with less than 95% MMR coverage, ten reported more than 5% of kindergartners had medical and nonmedical exemptions, highlighting the importance of targeted efforts at increasing vaccine confidence and access.
Recommendations for Healthcare Providers
Recommendations for Health Departments
Measles is an immediately notifiable disease. State, tribal, local, and territorial health departments have the lead in disease investigations and should report measles cases and outbreaks within 24 hours through the state health department to CDC (measlesreport@cdc.gov) and through NNDSS.
Recommendations for Parents and International Travelers
For More Information
Board of Directors – February 7, 2024 Meeting Minutes Read More »
Board of Directors – March 6, 2024 Meeting Minutes Read More »
The following content is from the FDA on March 8, 2024 and was not written by HVHD. Audience Product Certain live mussels from Allen’s Fisheries, Ltd. (NL0047SP), Benoit’s Cove, Newfoundland, Canada were initially harvested on 2/07/2024 (Julian date 24038) from harvest area AQ # 15 Newfoundland, with final harvest date of 2/18/2024 (Julian date 24049) and
The following content is from the FDA on March 8, 2024 and was not written by HVHD.
Certain live mussels from Allen’s Fisheries, Ltd. (NL0047SP), Benoit’s Cove, Newfoundland, Canada were initially harvested on 2/07/2024 (Julian date 24038) from harvest area AQ # 15 Newfoundland, with final harvest date of 2/18/2024 (Julian date 24049) and shipped to distributors in CT, FL, MD, MA, NJ, NY, and PA on or around 2/21/2024 (Julian Date 24052). The live mussels were distributed to restaurants and retailers in CT, FL, MD, MA, NJ, NY, and PA and may have been distributed to other states, as well.
The following product tag is provided to be representative of labeling that would accompany the implicated mussels.
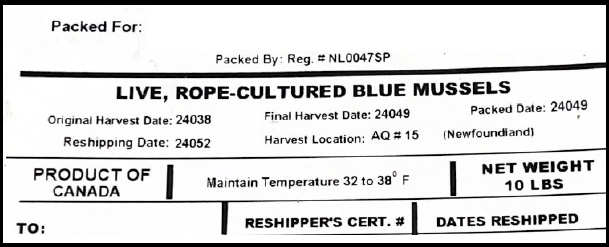
The FDA is advising restaurants and food retailers not to serve or sell and to dispose of mussels and consumers not to eat mussels from Allen’s Fisheries (NL0047SP) in Newfoundland, Canada, harvested on 2/07/2024 (Julian date 24038), from harvest area AQ # 15 Newfoundland, with final harvest date of 2/18/2024 (Julian date 24049) and shipped to distributors in CT, FL, MD, MA, NJ, NY, and PA on or around 2/21/2024 (Julian Date 24052) because they may be contaminated.
Contaminated shellfish can cause illness, especially if eaten raw, particularly in people with compromised immune systems. Food contaminated with pathogens or biotoxins may look, smell, and taste normal. Consumers of these products who are experiencing food poisoning symptoms such as diarrhea, stomach pain or cramps, nausea, vomiting, or fever should contact their healthcare provider, who should report their symptoms to their local Health Department.
On 3/1/2024, the New Jersey Department of Health advised the FDA of an outbreak of illness associated with consumption of certain mussels. The cases experienced symptoms including nausea, vomiting and diarrhea. The advisory includes mussels from Allen’s Fisheries (NL0047SP) in Newfoundland, Canada, harvested on 2/07/2024 (Julian date 24038), from harvest area AQ # 15 Newfoundland, with final harvest date of 2/18/2024 (Julian date 24049) and shipped to distributors in CT, FL, MD, MA, NJ, NY, and PA on or around 2/21/2024 (Julian Date 24052).
The FDA is issuing this alert advising restaurants and food retailers not to serve or sell and consumers not to eat mussels from Newfoundland, Canada, harvested on 2/07/2024 from harvest area AQ # 15 Newfoundland, with final harvest date of 2/18/2024, due to possible pathogen or biotoxin contamination. The FDA is awaiting further information on distribution of the mussels and will continue to monitor the investigation and provide assistance to state authorities as needed. As new information becomes available, the FDA will update the safety alert.
Restaurants and retailers should not serve or sell the potentially contaminated mussels. Restaurants and retailers should dispose of any products by throwing them in the garbage or contacting their distributor to arrange for return and destruction.
Restaurants and retailers should also be aware that shellfish may be a source of pathogens and should control the potential for cross-contamination of food processing equipment and the food processing environment. They should follow the steps below:
Consumers should not eat the potentially contaminated mussels. Consumers who have symptoms should contact their health care provider to report their symptoms and receive care.
To report a complaint or adverse event (illness or serious allergic reaction), you can:
Visit CFSAN’s Food & Cosmetic Information Center (FCIC) for additional consumer and industry assistance.
The following content is from the CT DPH on March 7, 2024 and was not written by HVHD. HARTFORD, Conn— The United States Food and Drug Administration has issued a public health alert regarding certain ground cinnamon products that contain levels of lead that exceed the federal lead content ban. The FDA is calling for a voluntary recall of the
High levels of lead found in numerous brands of ground cinnamon products Read More »
The following content is from the CT DPH on March 7, 2024 and was not written by HVHD.
HARTFORD, Conn— The United States Food and Drug Administration has issued a public health alert regarding certain ground cinnamon products that contain levels of lead that exceed the federal lead content ban. The FDA is calling for a voluntary recall of the following products:
The FDA said that it has sent a letter to all US cinnamon manufacturers, processors, distributors and facility operators to remind them of their obligation to prevent contamination. The agency also has expanded its testing to brands of ground cinnamon from discount retailers and analyzed those samples for lead and chromium.
“Consumers should not eat, use, sell or serve any of the ground cinnamon products listed here,” said Connecticut Department of Public Health Commissioner Manisha Juthani, MD. “If there is suspicion that someone has been exposed to elevated levels of lead, please talk to your health care provider. Symptoms from short-term exposure can include headaches, vomiting, and abdominal pain.”
Last fall, the FDA issued a similar alert about numerous applesauce products that were recalled due to the risk of elevated blood lead levels. Those items included WanaBana Apple Cinnamon Fruit Puree pouches, Schnucks brand Cinnamon-flavored Applesauce pouches, and Weis brand Cinnamon Applesauce pouches.
“It is critical to check your home for these products, which could be harmful if consumed,” added Connecticut Department of Consumer Protection Commissioner Bryan T. Cafferelli. “Just like with the applesauce recall, the team from the Department of Consumer Protection will work with retailers like SAV-A-LOT, Patel Brothers, Dollar Tree and Family Dollar to make sure these affected products are not on store shelves.”
For more information on the childhood lead program at DPH, please visit the program’s website. Connecticut residents can also reach out to their local health department if they have questions on lead poisoning prevention.